Inquest highlights role of guidelines
Dr Mark Woodrow, MBBS, MBA, GDipAppLaw, GCertArts, EMCert(ACEM), MACLM, General Manager – Medical Advisory Services, Avant
Thursday, 19 January 2023
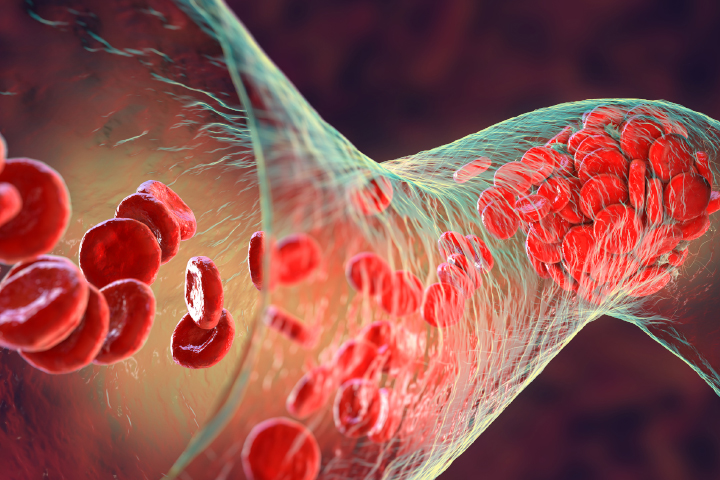
Doctors often face a delicate balance between slavishly following guidelines and using their clinical judgement. The tragic death of a young woman due to deep vein thrombosis (DVT) after minor surgery, reinforces that all patients should be assessed for venous thromboembolism (VTE) and the role of clinical guidelines.
The coroner said it was clear at the time of the inquest that the assessment and prevention of VTE was marked by “controversy and uncertainty”. From a medico-legal perspective, VTE is a foreseeable complication. Guidelines can assist doctors to navigate competing risks and can also be used when discussing the risks and benefits of treatments with patients.
Risk factors complicate fracture treatment
A 21-year-old female patient presented to a district hospital with a fractured and grazed left ankle after dancing in high heels.
The patient was a non-smoker and overweight, with a body mass index of about 35kg/m. She was also taking an oral contraceptive pill. She was given a tetanus booster and analgesics and started on intravenous antibiotics before being transferred to a tertiary hospital.
Her leg was considered too swollen for surgery, so a below-the-knee cast, analgesia and elevation were provided. Antibiotics were continued and the anticoagulant enoxaparin was administered for three days for DVT prophylaxis.
She was transferred to another hospital for the swelling to reduce and enoxaparin and her contraceptive pill were continued. At the time, the patient’s father told a staff member about his history of blood clots in the lungs and that he had been prescribed ongoing warfarin. He asked if his daughter would be given blood thinners and was told she was receiving them each night.
About two weeks later, she was transferred back to the tertiary hospital for surgery.
Discharged without anticoagulant
The patient's surgery was allocated to an orthopaedic registrar to perform an open reduction and internal fixation of the fracture. The patient was not given enoxaparin before surgery, and her chart shows she received enoxaparin in the evening following her surgery.
The inquest heard the usual practice at the hospital is that the orthopaedic surgeon who performs the surgery provides the post-operative instructions. As the usual practice was to consider a patient’s need for ongoing thromboprophylaxis at discharge, it was not surprising that the post-operative orders didn’t mention thromboprophylaxis.
A day after surgery, an on-call registrar reviewed the patient and discharged her after checking the post-operative instructions, which did not mention enoxaparin or aspirin. The patient was not asked about her family history of VTE or prescribed an anticoagulant.
Her father asked a doctor, who introduced himself as one of his daughter’s surgeons, whether she would be sent home with blood thinners. He was reportedly told, “No, her heart is good, she is young and strong like an ox.”
Cause of death
A month later, the patient saw her GP with shortness of breath, pleuritic chest pain and vomiting. She was sent to the emergency department of a general hospital, where she collapsed and suffered a cardiac arrest in the waiting room. Tragically, despite resuscitation efforts, she couldn’t be revived.
The coroner attributed her death to pulmonary embolism (PE) associated with DVT in her injured leg.
Inconsistent hospital guidelines
At the time, the hospital had two guidelines for thromboprophylaxis for lower limb trauma:
- The hospital’s guideline for fracture with immobilisation recommended enoxaparin starting six hours after surgery for the entire period of immobilisation.
- The orthopaedic department guideline, developed by the department based on the relevant literature, recommending the use of enoxaparin the morning after surgery, followed by 150 mg aspirin on discharge for patients with restricted weight bearing. For high-risk patients, enoxaparin was recommended six hours after surgery and warfarin for six weeks from the day after surgery.
The events involving this patient highlighted the discrepancy between the two sets of guidelines. At the time of the inquest, the hospital was taking steps to align the guidelines.
Differing views on DVT risk
Evidence presented at the inquest highlighted the challenge of managing patients with a moderate risk of DVT, and disagreement over whether the patient had a moderate or high-risk of DVT.
Expert evidence said risk factors for DVT included the oral contraceptive pill, lower limb fracture and being immobile. Family history was also very important and should always be considered during a risk assessment.
The expert opined that if the TIP (trauma, immobilisation and patient characteristics) risk score had been applied to the patient, she would have been classified high risk. Furthermore, enoxaparin would have reduced her risk by 60 to 80% and aspirin by 20 to 30%.
Coroner’s recommendations
Ultimately, the coroner accepted the decision not to prescribe prophylaxis was an omission rather than a failure of the guidelines.
However, while the coroner noted there was no guarantee the patient’s VTE would have been prevented had she been given prophylaxis, she was not treated in accordance with the hospital’s own guidelines. This exposed her to a much higher risk of developing a PE than would otherwise have been the case.
The coroner recommended implementing an effective assessment process throughout the state’s hospitals to prevent the risk of VTE, as far as practicable, and suggested considering the TIP score as part of this system.
The hospital’s reforms included introducing a VTE risk assessment eForm and developing a VTE information leaflet to give to all patients at risk of VTE.
Clinical guidelines and decision-making
As this inquest demonstrates, guidelines often come into play when experts are divided on what should have been done.
When deciding whether a doctor acted in a manner ‘widely accepted’ by peer professional opinion as competent practice, guidelines are important evidence of what was known and accepted at the time the care was provided.
The legal position is clear that ‘widely accepted’ does not mean ‘universally accepted.’ Widely held peer professional opinions can differ on what care should have been provided, yet still be viewed as competent and appropriate.
However, while guidelines provide recommendations for best practice, they should not replace clinical decision-making as they can vary and don’t always provide a clear consensus on treatment.
Ideally, guidelines are a tool doctors can use to help navigate competing risks such as the potential risk of VTE versus the risk of bleeding from VTE prophylaxis. They can also be used to assist in communicating the material risks and benefits of a treatment to patients to support informed consent and shared decision-making discussions.
Departing from guidelines
While courts recognise there may be a good reason for considered and rational departure from guidelines, if something goes wrong, the practitioner’s clinical reasoning will be scrutinised.
Generally, doctors who depart from standards of care based on their own unique views about treatment that are not supported by their peers, are more likely to fall foul of courts and tribunals.
In situations where you do depart from relevant guidelines, keep the following in mind:
- Consider whether your peers would agree that departing from the guidelines is appropriate in the patient’s circumstances.
- Carefully document your clinical reasoning for not following the guidelines in the records.
- If in doubt, consult your peers for their opinion.
Key lessons
- From a medico-legal perspective, VTE is a foreseeable complication of significance to the average patient.
- All patients should be assessed for VTE risk, given anticoagulant treatment if appropriate and provided with information about the potential risks of VTE and the risk of severe bleeding from VTE prophylaxis. These discussions should be documented in the patient’s clinical record.
- When deciding whether a doctor acted in a manner ‘widely accepted’ by peer professional opinion as competent practice, courts will rely on guidelines as evidence of what was known and accepted at the time the care was provided.
- Clinical guidelines are not a replacement for appropriate clinical decision-making and courts recognise there may be a good reason to depart from guidelines. In situations where you depart from the guidelines, carefully document your clinical reasoning in the records.
Related resources
Guidelines: The Australian Commission on Safety and Quality in Health Care’s Venous Thromboembolism Prevention Clinical Care Standard (2020) and Implementation Guide: Venous Thromboembolism Prevention Clinical Care Standard.
Avant article: Court finds following guidelines “not irrational.”
This article was originally published in Connect issue 19.
IMPORTANT: This article is not comprehensive and does not constitute legal or medical advice. You should seek legal or other professional advice before relying on its content, and practise proper clinical decision making with regard to the individual circumstances. Persons implementing any recommendations contained in this article must exercise their own independent skill or judgement or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant is not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published. © Avant Mutual Group Limited 2023.