
Conducting a telehealth consultation
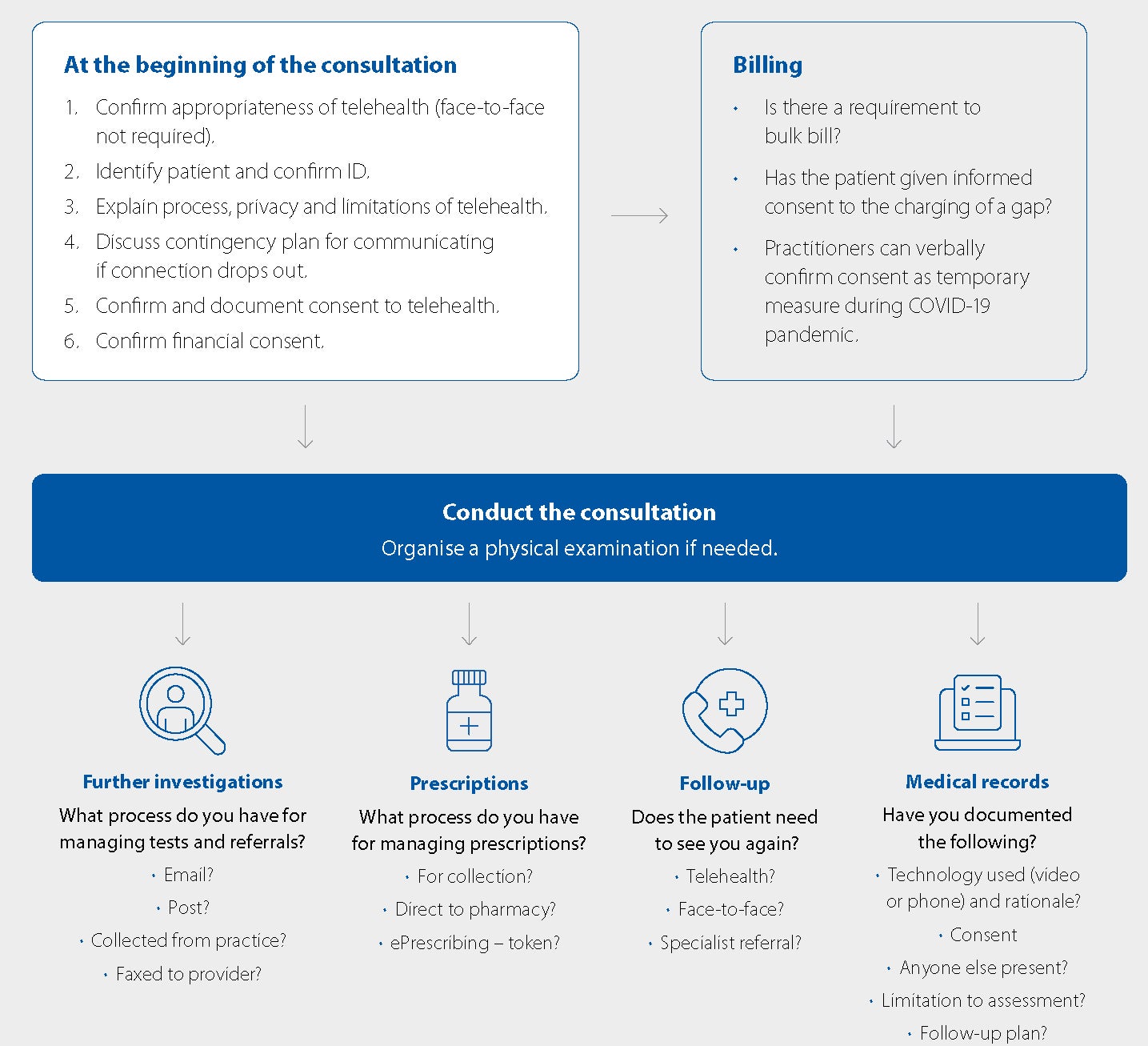
Summary: This checklist and flowchart outline the steps when conducting a telehealth consultation
Sunday, 1 November 2020
1. Preparation
The preparation required for a telehealth consultation is ideally supported by your practice staff and the appropriate policies. Have your staff:
- Confirm technology platform with patient and triage patient as appropriate for telehealth.
- Confirm and document consent to telehealth.
- Confirm financial consent.
As the practitioner:
- Access all the information you can from the medical records.
- Consider accessing the patient’s MyHealthRecord if available and appropriate.
2. Start the consultation
- Introduce yourself.
- Identify the patient and confirm their ID if you do not know them.
- Explain process and limitations of telehealth.
- Outline consultation process.
- Discuss a plan for technical trouble such as connection loss.
Privacy
- Give the patient some reassurance that their information through telehealth platform is safe and secure.
- Confirm that you are in a private setting and check their setting and who else may be present.
Consent
- Confirm consent to telehealth appointment.
- Confirm financial consent.
- Confirm consent to email/SMS.
- Discuss also the sharing of information with others in their care team.
Rapport
One of the challenges during a telehealth consultation is building the rapport needed for the patient to feel comfortable especially if they are not known to you. Consider the following tips:
- Keep a professional appearance.
- Minimise any potential distractions in view of the camera in your workspace. If you can, use picture in picture feature (e.g. where you can see both yourself and the patient) to see how you are being viewed by the patient, or if there is something distracting in the background (e.g., your cat!).
- Ensure your video is sufficiently “zoomed in” for the patient to see your facial expressions.
- Try to maintain good eye contact and a constant gaze into the camera, rather than frequently looking away at your computer or notes.
- Consider starting with a non-medical question. You may want to prepare a few questions to help engage with the patient.
- Increase your focus on basic communication skills such as active listening, not interrupting your patient and repeating back what you have heard. Delays experienced by the connection can make this especially important.
3. Conduct the consultation
Use strategies and evidence-informed practices to reflect the standard of care expected in a face-to-face consultation, as far as possible.
- Increase your emphasis on history taking and asking additional questions to compensate for reduced visual and physical clues.
- Check with the patient for any additional issues or concerns.
- Get the patient to confirm their understanding (e.g. ask them to repeat the information back to you).
Physical examination
There are obvious limitations to telehealth particularly in relation to physical examinations.
- Use the tools and resources you have or that the patient has at home (e.g. BP or blood sugar monitoring).
- Think laterally about what information you can glean virtually (e.g. functional assessments, information from the home environment).
- Support your patient to attend a face-to-face consultation where direct physical examination is required to continue providing good care.
Consent to treatment
If necessary, it is acceptable to consent a patient for a surgical procedure or other treatment or procedure via telehealth.
- Ensure the patient has plenty of opportunities to ask questions.
- Email supporting documentation to them such as information sheets.
- Advise them how to contact you if they have further questions.
Ongoing management
- Outline treatment plan.
- Discuss medications and side effects.
- Discuss importance of any further investigations, tests or referrals.
4. Close the consultation
- Check the patient’s preferred pharmacy/imaging/specialist.
- Agree on the plans for treatment.
- Outline to the patient how to get back in touch with you, or another practitioner and if needed discuss what they should do if symptoms change/get worse/don’t respond to treatment.
5. Documentation requirements
Documentation standards do not change when the consultation occurs virtually. However, there are additional things to document:
- What technology was used for the consultation (phone or video) and rationale.
- Whether patient has given financial consent.
- Whether the patient has consented to a telehealth consultation.
- Whether the patient has consented to being contacted by email.
- Whether anyone else was present.
- Whether there were any limitations to your assessment.
- Clinical reasoning, treatment and follow-up plans.
How to conduct a telehealth consultation
Still not sure about the correct order of steps to take? Here is a flow chart outlining how to conduct a telehealth consultation during COVID-19.
Useful resources
- Conducting a telehealth consultation flowchart
- Setting up telehealth in your practice factsheet
Disclaimers
This publication is not comprehensive and does not constitute legal or medical advice. You should seek legal or other professional advice before relying on any content, and practise proper clinical decision making with regard to the individual circumstances. Persons implementing any recommendations contained in this publication must exercise their own independent skill or judgement or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant is not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published. [November 2020]